Insights and Introductions: Meet the 2025–2026 Presidential Fellows in Collaborative Neuroscience

The University of Virginia is proud to announce the 2025–26 cohort of Presidential Fellows in Collaborative Neuroscience. Fellows will receive funding and mentorship to pursue high-impact research projects that advance our understanding of the brain and nervous system. The Fellowship program underscores UVA’s commitment to fostering interdisciplinary research and cultivating the next generation of scientific leaders.
In the following Q&A, meet the people behind the research—what drives their curiosity, the challenges they’re tackling, and their visions for the future of neuroscience.
Reza Ghorbani, Electrical & Computer Engineering
Mentors: Merry Mani and Mathews Jacob

Q: Describe your research in seven words.
A: Imaging to detect neurodegeneration for early treatment.
Q: What inspired you to pursue this area of neuroscience?
A: My inspiration stems from a deep understanding of the societal burden posed by neurodegenerative disorders, such as Alzheimer's and Parkinson's disease. As a medical imaging engineer, recognizing the limitations of current diagnostics and interventions motivated me to develop advanced imaging methods to detect early-stage neuronal changes before irreversible damage occurs. In particular, diffusion magnetic resonance imaging (dMRI), which measures water displacement at micron scales, promises a physics-based window to study the microstructural change years before clinical symptoms are detected.
My goal is to push this technology to its full potential: faster, higher-resolution imaging that enables clinicians to identify these conditions when they’re still treatable. It’s where my technical expertise and my desire for clinical impact converge.
Q: What are the potential impacts of your research?
A: My research has the potential to significantly transform clinical practice by enabling early diagnosis of neurodegenerative disorders through advanced diffusion MRI techniques. By providing precise, compartment-specific biomarkers at an unprecedented resolution, this technology could improve early intervention strategies, accelerate clinical trials for new therapies, and enhance personalized treatment plans, thus directly benefiting patient health and healthcare efficiency. Moreover, the ability to detect compartment-specific biomarkers can benefit studies of neurobiology models by providing a better understanding of the pathological cascade of neurodegeneration.
Future directions include validating the biomarkers across larger patient cohorts, exploring additional neurodegenerative conditions, and integrating emerging technologies like ultra-high-performance gradient systems and advanced multi-dimensional diffusion encoding. These developments will deepen our understanding of early disease processes, refine diagnostic capabilities, and inform targeted therapeutic strategies.
Over the next few years, I envision my research expanding to incorporate increasingly sophisticated machine learning algorithms and ultra-high-resolution imaging techniques.
Piotr Kraszewski, Neuroscience
Mentors: Elise Cope and Sarah Flowers

Q: Describe your research in seven words.
A: Perineuronal net sulfation influence on social memory.
Q: What are the potential impacts of your research?
A: If successful, my research could pinpoint novel targets to treat social memory deficits prevalent in Alzheimer’s disease, potentially increasing patients’ healthspan.
Q: How do you see your research evolving over the next few years?
A: I believe that in the coming years, perineuronal nets will continue to gain attention as key modulators of memory. Progress in this field has been slowed in part by a lack of tools to study their composition and to manipulate specific components. However, the development of spatial glycoproteomics promises to overcome this barrier by enabling more precise identification of disease-related changes in perineuronal net composition—including at the protein, carbohydrate, and sulfation levels.
Additionally, with the development of inhibitors targeting enzymes involved in glycosaminoglycan synthesis, it may become feasible to non-invasively modulate perineuronal net composition to ultimately mitigate social memory dysfunction in Alzheimer’s disease patients.
Zhenyu Lei, Electrical & Computer Engineering
Mentors: Jundong Li and Aiying Zhang

Q: Describe your research in seven words.
A: Interpretable AI models decoding human brain connectivity.
Q: What inspired you to pursue this area of neuroscience?
A: With the development of AI tools, they have been widely utilized by researchers to solve neuroscience related problems. However, these AI tools are usually black-box, leaving them less reliable and providing limited insights. As a result, I would like to explore using explainable AI to unveil those myths underlying the AI’s superpower in solving neuroscience problems, and hopefully to uncover insights that can benefit interdisciplinary research.
Q: What are the potential real-world impacts of your research and how do you see your research evolving over the next few years?
A: By successfully identifying the critical attention-related neuro-circuits that drives attention dysfunction with explainable AI, we can provide insights for medical researchers to design interventions that can be translated into improved clinical outcomes in curing attention-related deficiencies. We hope a lot of children with attention dysfunction can benefit from our project. I think I would keep focusing on using AI tools to reliably solve different kinds of brain-related disease with better explanations. It would be very interesting to explore if there is a generalized foundation model that can be applied to all kinds of brain disease, where I believe that such models can bring huge insights for the connection of different kinds of disease and true cause of those diseases.
Kaela Lettieri, Cell & Developmental Biology
Mentors: Noelle Dwyer and Stefanie Redemann

Q: Describe your research in seven words.
A: Investigating how disrupted cell division affects neurodevelopment.
Q: What inspired you to pursue this area of neuroscience?
A: Building a brain of the proper size and structure is a complicated process. Neural stem cells (NSCs) need to undergo precisely timed divisions to produce enough neurons to build the brain, and disruptions to this process can lead to severe brain malformations.
Although I have always been interested in neuroscience, I became fascinated with how the smallest disruption to NSC divisions have such an immense impact on the developing brain. Therefore, I wanted to continue to investigate how disruptions to this process affect development to uncover avenues for potential treatments to prevent these severe brain malformations.
Q: What are the broader implications of your research, and how do you envision it developing in the coming years?
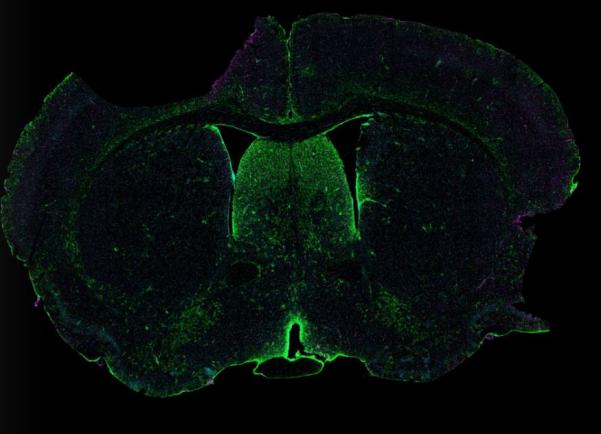
A: Proper proliferation of neural stem cells (NSCs) during development is essential for building an appropriately sized brain. In the last step of cell division, abscission of the cytokinetic midbody (MB) connecting the two daughter cells is critical for proper cell fates and structure, with disruptions to this process resulting in severe brain malformations in humans. The MB remnant, the piece of MB left over after abscission, has been suggested to serve as an extracellular vesicle that influences cell fate upon binding or engulfment and contains thousands of proteins involved in various processes throughout the cell. My proposed project involves isolating the MB remnants from NSCs to examine the protein contents which will lead to new avenues of investigation by uncovering novel proteins specifically involved in cytokinetic abscission of the brain. This will allow for new studies examining the function of these proteins and how loss of these proteins affect NSC cytokinetic abscission.
Julianna Mollica, Constructed Environment
Mentors: Andrew Mondschein, Nicole Long, and Michael Sheehy

Q: Describe your research in seven words.
A: Investigating how environments influence stress and perception.
Q: What inspired you to pursue this area of neuroscience?
A: I'm deeply interested in how the built environment can support mental health and wellbeing across the lifespan. While architecture often addresses physical needs through elements like air quality or accessibility, mental health remains relatively understudied. My work explores how biophilic design influences stress regulation, combining neuroscience methods like EEG with other physiological and behavioral measures to build a more holistic understanding of environmental effects on health. What excites me most about environmental neuroscience is not only its potential to deepen our understanding of human–environment interactions, but also its real-world relevance: empirical insights can inform design, planning, and policy to promote healthier spaces.
Q: What are the potential impacts of your research?
A: I hope to demonstrate that relatively fundamental design elements, like access to nature or the use of natural materials, can have a significant impact on mental health and wellbeing. This research can help inform evidence-based design practices for architects and related disciplines. With robust and consistent findings, this work could strengthen the case for treating mental health as a design priority, not an afterthought. Certain decisions shouldn’t be seen as luxuries, but as essential to supporting psychological functioning and overall mental wellbeing. Ultimately, I want this kind of human-centered design to become the new baseline, especially in settings where it matters most, like affordable housing.
Lizzie Zhang, Neuroscience
Mentors: Edward Nieh and Wendy Lynch

Q: Describe your research in seven words.
A: Using sugar and cocaine to study addiction.
Q: What has been the most exciting or surprising finding in your work so far?
A: The most striking finding has been observing how dramatically our head-fixed mice prioritize cocaine over sucrose when both rewards are simultaneously available. This contradicts findings from other laboratories where rodents typically prefer sucrose over cocaine. What makes this particularly exciting is that our protocol appears to successfully recapitulate a hallmark feature of human addiction—the pathological prioritization of drug rewards over natural rewards like food and social interaction. This behavioral shift suggests we're capturing a critical aspect of addiction that may have been missed in most of previous models, potentially providing a more clinically relevant platform for understanding the neural mechanisms underlying substance use disorders.
Q: What are the potential impacts of your research?
A: Currently, there are no FDA-approved medications specifically for cocaine use disorder, leaving clinicians to rely primarily on behavioral and psychological interventions that unfortunately yield inconsistent treatment outcomes. Our research has the potential to identify novel therapeutic targets by revealing the specific neural populations and mechanisms that drive the transition from natural reward preference to drug reward prioritization. By understanding how hippocampal CA1 neurons differentially encode these reward types, we could develop precision medicine approaches that selectively modulate drug-seeking circuits while preserving natural reward processing. This could lead to pharmacological interventions that restore healthy reward hierarchy, offering hope for the millions struggling with cocaine addiction who currently have limited effective treatment options.